contact us
- Contact Us
- +26 0 211 242 257
- http://www.cidrz.org
Toolkit for Implementing and Evaluating Differentiated Service Delivery Models to Improve HIV Treatment Outcomes
Both health systems and job aides should be prepared to support implementation of DSD models.
The World Health Organization (WHO) states that “A health system consists of all organizations, people and actions whose primary interest is to promote, restore or maintain health.” The Differentiated Care website also offers elements to consider when make adjustments in the health system building blocks that may be needed for successful implementation of DSD model. Below we provide some suggestions for health system adjustments based on WHO building blocks. DSD model-specific steps are provided in [link to next main navigation tool]
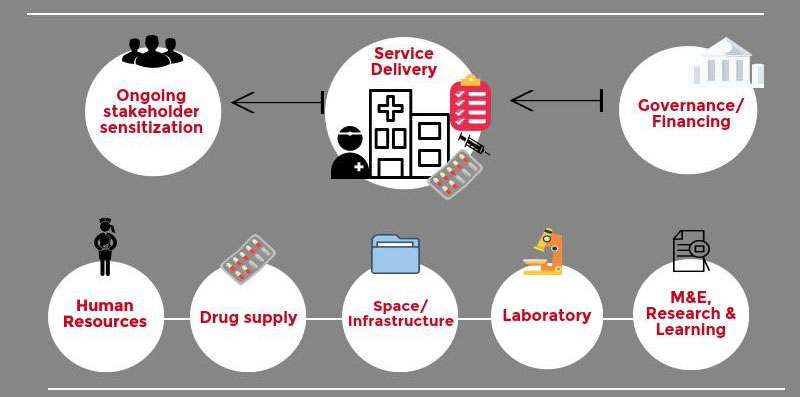
Leadership and Governance provide the necessary strategic DSD policy frameworks in combination with effective oversight, coalition-building, the provision of appropriate regulations and incentives, attention to system-design, and accountability.
The health financing system must raise adequate funds to ensure that people can use needed DSD services, and are protected from financial catastrophe or impoverishment associated with having to pay for them.
DSD must follow the principles of good health service delivery to deliver effective, safe, quality personal and non-personal health interventions to those who need them, when and where needed, with minimum waste of resources.
Ongoing stakeholder sensitization through upfront and ongoing engagement of key players involved in service and delivery, requires effective communication on programs, progress updates, and feedback. Key stakeholders for DSD include Ministries of Health, health care workers, patients, community members, chiefs, other community leaders, and any other individual who may be identified as key to programmatic success.
The health workforce should consist of sufficient numbers and mix of DSD staff, who are provided with the training, skills and tools needed to ensure that they are competent, responsive and productive.
Patients enrolled into DSD models should have equitable access to antiretroviral drugs, essential medical products, vaccines and technologies of assured quality and based on scientific evidence of safety, efficacy and cost-effectiveness.
Space and Infrastructure may need remodeling to accommodate new patient flows for patients enrolled in DSD models.
Laboratory services, schedules and filing systems may need changes to gain efficiencies and to ensure that routine tests and results are provided to patients.
Monitoring and Evaluation and Research and Learning (MERL) are important to gain health information and make evidence-based decisions. Indicators to monitor progress must be decided to have information needed to make midcourse changes. Long-term systematic and objective assessment will provide the information needed to assess program success. Ongoing research is necessary to ensure patient needs are understood and met, that the program is safe, efficacious and effective. Lessons learned should be incorporated into ongoing practices to increase effectiveness and sustainability over time. Learning includes sharing best practices and lessons learned both internally and externally. Learn more
In order for DSD models to function, it is important to think about what tools and structures are needed.

Questions to ask yourself
Establish eligibility for DSD enrolment:
Who is / should be eligible to participate in DSD models?
Use WHO and country guidelines to determine eligibility for enrolment into each DSD model.
Are there other considerations? Learn More
Identify DSD program inputs:
What inputs are required for DSD models to function?
Some program inputs include:
Develop DSD training toolkit:
What training materials are needed?
Adapt existing training materials to the local context. [Link to our training materials]
Develop DSD Standard Operating Procedures:
What are the standard operating procedures once DSD models are implemented?
Standard operating procedures for enrolment into models and ongoing DSD model programming is key to ensuring staff know their roles and responsibilities within DSD. Our training materials can be adapted to create standard operating procedures.
Train Program Staff:
Which staff must be provided training?
Staff need to be trained in DSD in order to ensure a smooth transition from routine care. Training is provided using training materials and standard operating procedures with necessary practical activities such as obtaining dry blood spots for viral load.
Key stakeholder sensitization:
Which stakeholders should be approached?
Engaging and communicating with MoH at national, provincial and district levels; health care providers, patients, community members and leaders is key to buy-in and DSD success. Having correct information about services reduces risk of incorrect knowledge spreading.