April 26, 2024
Meet Hillary Hanaimaila, a brilliant psychosocial counsellor working under the Centre for Infectious Disease Research in Zambia (CIDRZ)’s CDC-funded Common Elements Treatment Approach (CETA) programme stationed […]
April 25, 2024
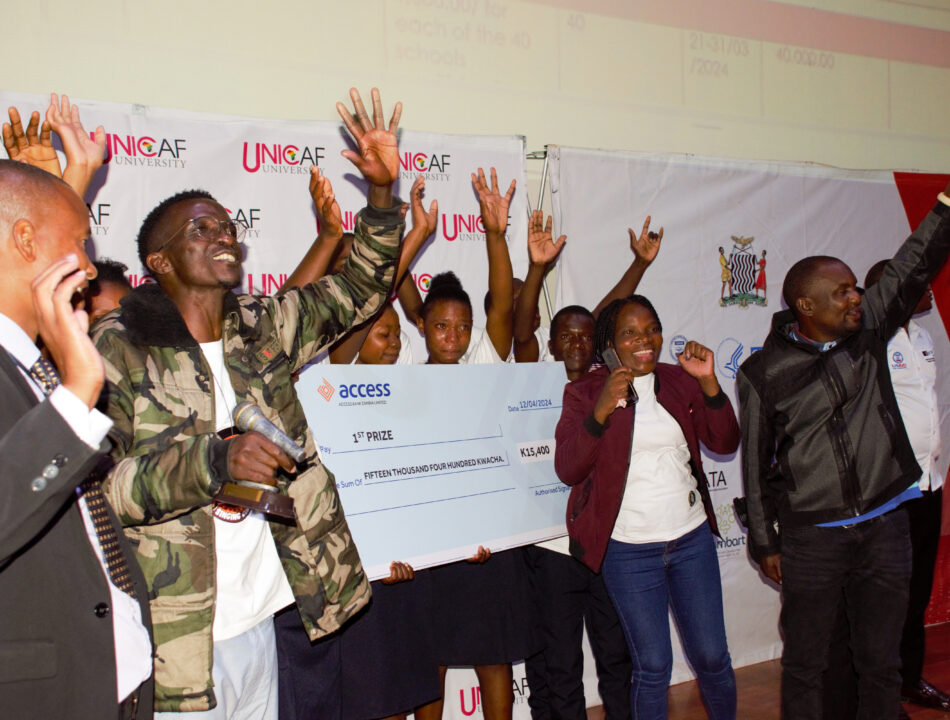
The Zambia Monitoring and Evaluation Association recently convened its highly anticipated Symposium and General Meeting, an event that enabled M&E professionals to exchange and highlight the […]
April 22, 2024
The World Health Organisation (WHO) has commended Zambia for its proactiveness in tackling cancer. A delegation from the WHO led by Dr Bente Mikkelsen, Director of […]