CIDRZ Highlights Gaps in Maternal HIV Retesting at 16th Annual HIV/TB/STI/Viral Hepatitis Conference.
December 12, 2024
CIDRZ, LPHO Host Meeting to Strengthen PMTCT Programme in Lusaka
December 17, 2024Silent transfers in HIV care represent a significant challenge to public health and the continuity of treatment for individuals with HIV. Silent transfers occur when people receiving antiretroviral therapy (ART) enroll in a new healthcare facility without disclosing their treatment history, which can disrupt treatment and inadvertently impair their health.
To address this challenge, the Centre for Infectious Disease Research in Zambia (CIDRZ) conducted a study exploring the root causes of silent transfers, identifying systemic gaps, and proposing actionable solutions.
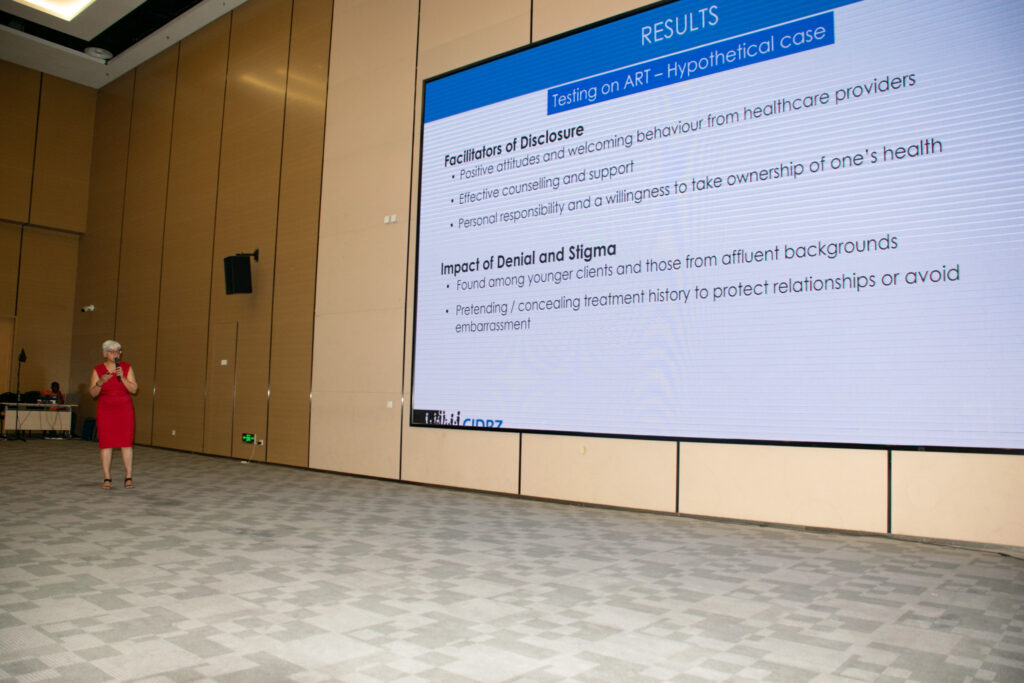
CIDRZ’s Dr Anjali Sharma presented the findings at the 16th Annual National HIV/TB/STI/Viral Hepatitis Conference in Lusaka, explaining that fear of judgment, stigma, or breaches of confidentiality, particularly in settings where individuals might encounter acquaintances, serves as a significant barrier to disclosure.
She further highlighted that this pervasive fear often leads individuals to withhold treatment history, which deepens challenges to continuity of care.
The study revealed that anxiety and emotional distress also play a critical role, with denial of HIV status and apprehension about partner reactions contributing to repeat HIV testing and non-disclosure.
It further outlined that logistical hurdle such as missing transfer documents and long wait times, intensify the problem. Many people feel uneasy about navigating the healthcare system due to complex and unclear transfer processes.
The study also identified several supportive practices among healthcare providers, such as maintaining confidentiality, fostering communication, and demonstrating empathy to build a person-centred healthcare environment. However, some shortcomings within the healthcare system, such as complex and poorly communicated transfer processes, discourage individuals from officially transferring their records, resulting in unnecessary retesting. Additionally, insufficient staffing and inadequate infrastructure, such as a lack of private consultation spaces, compromise the delivery of person-centred care.
The study recommends community sensitization to raise awareness about patients’ rights, the importance of accurate medical histories, and the benefits of disclosure. Simplifying and streamlining patient transfer processes is essential for improving continuity of care. Structural improvements, such as enhancing private consultation spaces, also foster privacy and build trust between patients and healthcare providers.
This study underscores the importance of adopting a person-centred approach to HIV care. The healthcare system can create an environment where people feel supported and valued, by addressing stigma, simplifying processes, and empowering both individuals and healthcare providers.